Reports
When will the COVID-19 pandemic end?, McKinsey & Company
A world wearied by the First World War and sickened by the 1918 flu pandemic desperately sought to move past the struggles and tragedies and start to rebuild lives. People were in search of a “return to normalcy,” as Warren G. Harding put it. Today, nearly every country finds itself in a similar position.
More than eight months and 900,000 deaths into the COVID-19 pandemic,1 people around the world are longing for an end. In our view, there are two important definitions of “end,” each with a separate timeline:
- An epidemiological end point when herd immunity is achieved. One end point will occur when the proportion of society immune to COVID-19 is sufficient to prevent widespread, ongoing transmission. Many countries are hoping that a vaccine will do the bulk of the work needed to achieve herd immunity. When this end point is reached, the public-health-emergency interventions deployed in 2020 will no longer be needed. While regular revaccinations may be needed, perhaps similar to annual flu shots, the threat of widespread transmission will be gone.
- A transition to a form of normalcy. A second (and likely, earlier) end point will occur when almost all aspects of social and economic life can resume without fear of ongoing mortality (when a mortality rate is no longer higher than a country’s historical average) or long-term health consequences related to COVID-19. The process will be enabled by tools such as vaccination of the highest-risk populations; rapid, accurate testing; improved therapeutics; and continued strengthening of public-health responses. The next normal won’t look exactly like the old—it might be different in surprising ways, with unexpected contours, and getting there will be gradual—but the transition will enable many familiar scenes, such as air travel, bustling shops, humming factories, full restaurants, and gyms operating at capacity, to resume.
The two ends are related, of course, but not linearly. At the latest, the transition to normal will come when herd immunity is reached. But in regions with strong public-health responses, normalcy can likely come significantly before the epidemiological end of the pandemic.
The timeline to achieve the ends will vary by location. In this article, we’ll explain the criteria that will be key factors in determining when each is reached. In the United States and most other developed economies, the epidemiological end point is most likely to be achieved in the third or fourth quarter of 2021, with the potential to transition to normalcy sooner, possibly in the first or second quarter of 2021. Every day matters. Beyond the impatience that most feel to resume normal life, the longer it takes to remove the constraints on our economies, the greater will be the economic damage.
The epidemiological end point
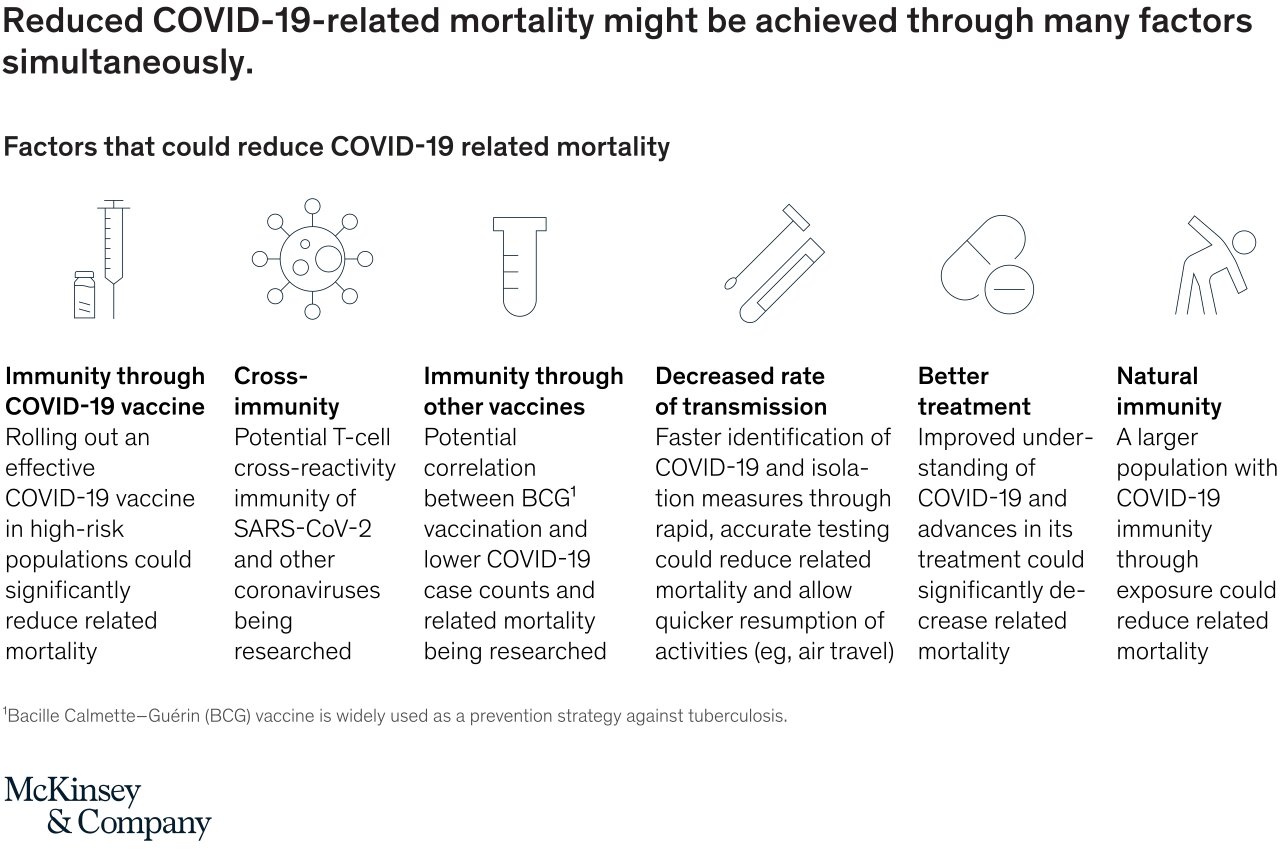
Most countries have deferred the hope of achieving herd immunity until the arrival of a vaccine. When herd immunity is reached, ongoing public-health interventions for COVID-19 can stop without fear of resurgence. The timing of the end point will vary by country and will be affected by a number of factors:
- the arrival, efficacy, and adoption of COVID-19 vaccines—the biggest drivers in the timeline to herd immunity2
- the level of natural immunity in a population from exposure to COVID-19; in our estimate, between 90 million and 300 million people globally may have natural immunity3
- potential cross-immunity from exposure to other coronaviruses4
- potential partial immunity conferred by other immunizations, such as the bacille Calmette–Guérin (BCG) vaccine for tuberculosis5
- regional differences in the ways that people mix, which will produce different thresholds for herd immunity
Consider the first and most crucial variables: the arrival of vaccines, their efficacy, and their adoption. We see four plausible scenarios for vaccine efficacy and adoption, illustrated in Exhibit 1.Different combinations of those two factors will drive varying levels of conferred immunity, implying the extent of natural immunity that will be required to reach herd immunity under each scenario. Combinations of efficacy and adoption beyond those shown are possible.

The other variables will also have much to say about the timeline to reach herd immunity (see sidebar, “Key factors affecting the timeline to herd immunity”).
Based on our reading of the current state of the variables and their likely progress in the coming months, we estimate that the most likely time for the United States to achieve herd immunity is the third or fourth quarter of 2021. As we wrote in July 2020, one or more vaccines may receive US Food and Drug Administration Emergency Use Authorization before the end of 2020 (or early in 2021) and the granting of a Biologics License Application (also known as approval) during the first quarter of 2021.
Vaccine distribution to a sufficient portion of a population to induce herd immunity could take place in as few as six months. That will call for rapid availability of hundreds of millions of doses, functioning vaccine supply chains, and peoples’ willingness to be vaccinated during the first half of 2021. We believe that those are all reasonable expectations, based on public statements from vaccine manufacturers and the results of surveys on consumer sentiment about vaccines.7
Herd immunity could be reached as soon as the second quarter of 2021 if vaccines are highly effective and launched smoothly or if significant cross-immunity is discovered in a population (Exhibit 2). (For more on the potential for a faster resolution of the COVID-19 crisis in the United States, see “Searching for optimism in the US response to COVID-19,” forthcoming on McKinsey.com.) On the other hand, the epidemiological end of the pandemic might not be reached until 2022 or later if the early vaccine candidates have efficacy or safety issues—or if their distribution and adoption are slow. At worst, we see a long-tail possibility that the United States could be still battling COVID-19 into 2023 and beyond if a constellation of factors (such as low efficacy of vaccines and a short duration of natural immunity) align against us.

The paths to herd immunity in other high-income countries are likely to be broadly similar to the one in the United States. The timelines will vary based on differences in vaccine access and rollout and in levels of natural immunity—and potentially, in levels of cross-immunity and previous coverage of other vaccines, such as the BCG vaccine. Even as some locations reach herd immunity, pockets of endemic COVID-19 disease are likely to remain around the world, for example in areas affected by war or in communities with persistently low adoption of vaccines. In such places, until herd immunity is reached, COVID-19 might be analogous to measles—not a day-to-day threat to most people, but a persistent risk. If immunity wanes—for example, if booster vaccines are not fully adopted—then COVID-19 could become more widely endemic.
The arrival of herd immunity won’t mean a complete end to all public-health interventions. It’s possible that regular revaccinations would be required to maintain immunity, and ongoing surveillance for COVID-19 will be required. But herd immunity would mean that the emergency measures currently in place in many countries could be lifted.
The pace at which governments relax public-health measures will be critical. Some of those measures (such as full lockdowns and restrictions on certain industries) have significant social and economic consequences, and others (such as testing and tracing), while expensive, don’t. Many governments are employing packages of measures that aim to minimize the number of COVID-19 cases and excess mortality while maximizing social and economic degrees of freedom.
The transition to normal
The second end point of the pandemic may be reached earlier than the first. We estimate that the mostly likely time for this to occur is the first or second quarter of 2021 in the United States and other advanced economies. The key factor is diminished mortality.
Society has grown used to tracking the number of COVID-19 infections (the case count). But case counts matter primarily because people are dying from the disease and because those who survive it may suffer long-term health consequences after infection. The latter is an area of scientific uncertainty, but there is concern that some recovered patients will face long-term effects.8
Most countries have made significant progress in reducing the numbers of deaths and hospitalizations associated with COVID-19. Some are close to eliminating excess mortality. Those results have generally been achieved through a combination of moderately effective interventions rather than a single “big bang” (Exhibit 3).
A transition to the next normal, in whatever form that takes, will come gradually when people have confidence that they can do what they used to do without endangering themselves or others. Gaining that confidence will require a continuation of the progress made to reduce mortality and complications, as well as further scientific study regarding long-term health consequences for recovered patients. When confidence is restored, people will again fill bars, restaurants, theaters, and sports venues to full capacity; fly overseas (except for the highest-risk populations); and receive routine medical care at levels similar to those seen prior to the pandemic.
The timing of such a transition will depend on the progress toward herd immunity, as previously detailed (since more people with immunity means fewer deaths and long-term health consequences), and on the effectiveness of a country’s public-health response. Transitions will be gradual. They have already begun in some locations and could be well advanced in most countries by the first or second quarter of 2021. Given the interconnectedness of the global economy, country timelines to normalcy are not fully independent of one another.
To achieve that, we will need to see significant progress on the epidemiological end point, including an effective vaccine receiving Emergency Use Authorization approval during the fourth quarter of 2020 or the first quarter of 2021, followed by a smooth rollout and adoption by high-risk populations. Favorable findings on natural and cross-immunity would help accelerate timelines. Five additional criteria will also contribute to the transition to a form of normalcy—the more of these that are achieved, the faster the milestone is likely to be reached:
- continued improvement by governments in the application of public-health interventions (such as test and trace) that don’t significantly limit economic and social activities
- compliance with public-health measures until we achieve herd immunity
- accurate, widely available, rapid testing that effectively enables specific activities
- continued advancements in therapeutics (including pre- and postexposure prophylactics) for and clinical management of COVID-19, leading to lower infection-fatality ratios—substantial progress has already been made through a combination of effective drugs, such as dexamethasone and remdesivir, and changes in clinical management
- public confidence that there aren’t significant long-term health consequences for those who recover from COVID-19
Both the epidemiological and normalcy ends to the COVID-19 pandemic are important. The transition to the next normal will mark an important social and economic milestone, and herd immunity will be a more definitive end to the pandemic. In the United States, while the transition to normal might be accomplished sooner, the epidemiological end point looks most likely to be reached in the second half of 2021. Other advanced economies are probably on similar timetables. McKinsey & Company













You must be logged in to post a comment Login